Michael C. Spaeder, MD, MS

 Dr. Spaeder’s somewhat unusual background in mathematics and statistics has greatly informed his research pursuits. Prior to his medical training, he completed graduate studies in mathematical statistics at the George Washington University and was employed as a statistical consultant with the Economics Consulting and Quantitative Analysis group at Ernst & Young, LLP in Washington, DC. In his medical research career, he has sought to bridge his foundation in mathematics and statistics with his clinical focus, caring for critically ill and injured infants and children in the pediatric intensive care unit (PICU).
Dr. Spaeder’s somewhat unusual background in mathematics and statistics has greatly informed his research pursuits. Prior to his medical training, he completed graduate studies in mathematical statistics at the George Washington University and was employed as a statistical consultant with the Economics Consulting and Quantitative Analysis group at Ernst & Young, LLP in Washington, DC. In his medical research career, he has sought to bridge his foundation in mathematics and statistics with his clinical focus, caring for critically ill and injured infants and children in the pediatric intensive care unit (PICU).
Predictive Monitoring in the PICU
Children and infants in PICUs often deteriorate suddenly due to sub-acute potentially catastrophic illness. Standard around-the-clock bedside monitoring of physiologic parameters, which might give clues about incipient deterioration, often flies by unnoticed. To solve this problem of undetected changes, predictive monitoring integrates these data to give clinicians early warning of events, allowing earlier, more effective intervention.
he Center for Advanced Medical Analytics at UVA is a national leader is the creation and implementation of predictive modeling algorithms of clinical deterioration in critically ill patients. These algorithms often work through the analysis of the behavior of certain physiologic parameters (e.g. heart rate variability). Often coupled with data extracted from the electronic health record, individualized patient stability indices can be calculated, allowing for early identification of at-risk patients. Dr. Spaeder is leading the effort to build predictive algorithms of sepsis and shock for infants and children in the PICU.
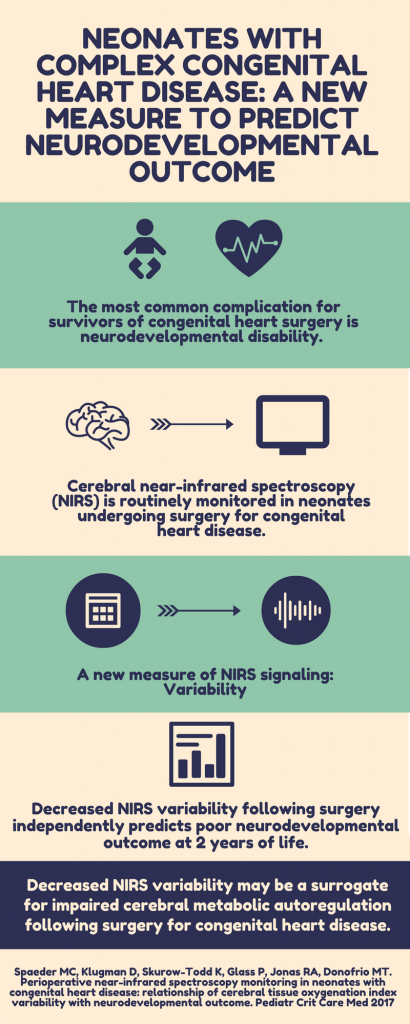
Recently, Dr. Spaeder has been engaged in investigations of the use of near infrared spectroscopy (NIRS) as a predictive monitoring tool for neonates undergoing surgery for congenital heart disease. He has proposed a new measure of NIRS signaling, variability of regional tissue oxygenation. His hypothesis is that reduced regional tissue oxygenation variability as measured by NIRS is a surrogate for impaired autoregulation or inadequacy of compensatory mechanisms. He has tested this hypothesis on two different cohorts of neonates undergoing surgery for congenital heart disease to predict low cardiac output syndrome in the short term and poor neurodevelopmental outcomes in the long term. He expects to undertake work in the near future to correlate cerebral NIRS variability with different perfusion strategies during cardiopulmonary bypass and with microstructural and metabolic abnormalities detected by neuroimaging.
